Analysis of breast true-cut biopsies by applying immunohistochemical study of myoepithelial markers
Main Article Content
Abstract
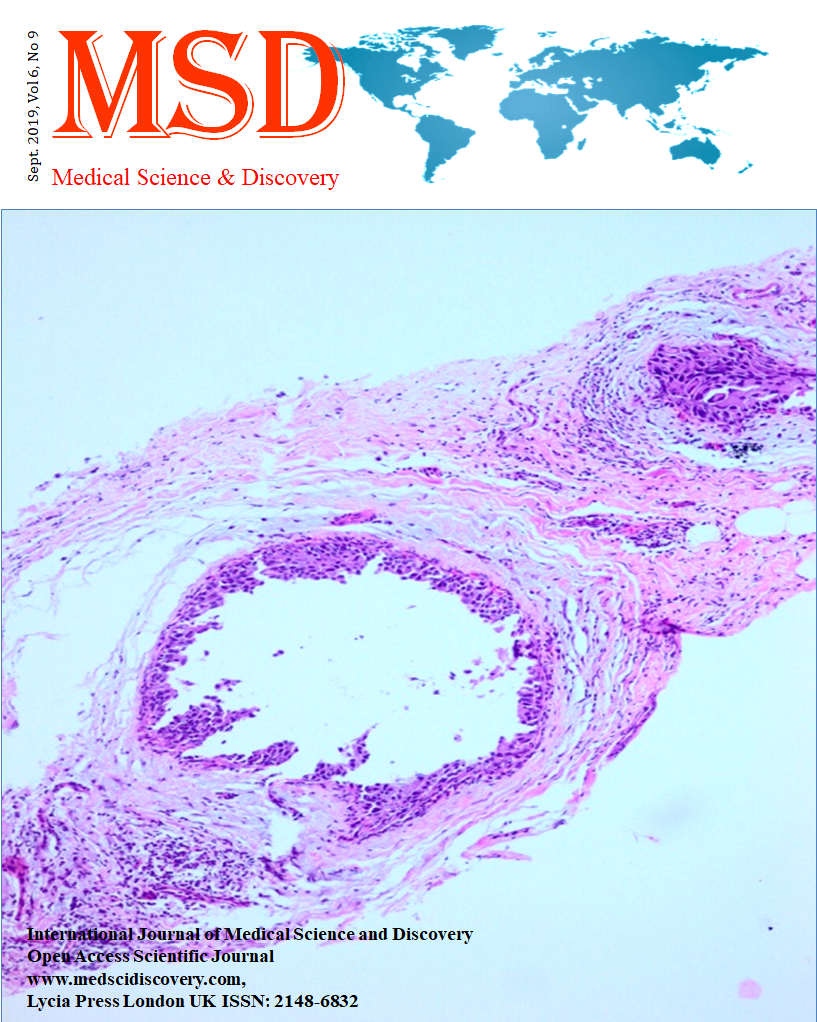
Objective: Breast pathologies are very common in women. Breast cancer is the most common and most frequent cause of death in women. The most common type of breast cancer is invasive ductal carcinoma. Histopathological examination of the tissue taken with a fine needle aspiration biopsy or true-cut biopsy is the main diagnostic method when clinical examination of breast and/ or radiological mass is detected. The definitive diagnosis of benign and malignant lesions of the breast is important in the form of treatment. The most important features in the diagnosis of breast cancer are atypical cellular features such as invasion, desmoplasia, pleomorphism, hyperchromasia, nuclear irregularity, prominent nucleoli, high mitosis count. Loss of myoepithelial layer in the malignant cases is a very important feature in the diagnosis. Aim of this study is to evaluate the benign and malignant breast pathologies with the immunohistochemical panel.
Material and Methods: 52 breast true-cut biopsy materials in the archives of Department of Pathology at Faculty of Medicine, Erzincan Binali Yıldırım University between 2015-2017 were re-examined with the immunohistochemical panel. The immunohistochemical staining markers such as estrogen, progesterone, cerb-B2, E-cadherin, P63, CD10, calponin, CK5/6 have been applied in all cases.
Results: 23 cases were a benign disease such as fibroadenoma, adenosis, fibrosis, fibrocystic changes, and intraductal papilloma. 29 cases were a malignant epithelial tumor.
Conclusion: In the diagnosis of breast cancers, mainly cellular properties are determinative. The evaluation with the immunohistochemical panel will reduce the risk of diagnostic error when the cases that difficultly diagnosed with cellular properties.
Downloads
Article Details
Accepted 2019-09-05
Published 2019-09-09
References
2. Figueroa JD, Pfeiffer RM, Brinton LA, Palakal MM, Degnim AC, Radisky D et al. Standardized measures of lobular involution and subsequent breast cancer risk among women with benign breast disease: a nested case-control study. Breast Cancer Research & Treatment 2016;159(1):163-72.
3. Chang JM, Moon WK, Cho N, Yi A, Koo HR, Han W, et al. Clinical application of shear wave elastography (SWE) in the diagnosis of benign and malignant breast diseases. Breast Cancer Res Treat. 2011 Aug;129(1):89-97.
4. Greenberg R, Skornick Y, Kaplan O. Management of breast fibroadenomas. J Gen Intern Med. 1998 Sep; 13(9):640-5.
5. Chen YL, Chen JJ, Chang C, Gao Y, Wu J, Yang VT,et al. Sclerosing adenosis: Ultrasonographic and mammographic findings and correlation with histopathology. Molecular and Clinical Oncology. 2017;6:157-62.
6. Tavassoli FA. Pathology of the breast. Norwalk: Appleton and Lange, 1992;93-7.
7. What is breast cancer? Imaginis. 2008. Jun 11, [17 Mar 2010]. http://www.imaginis.com/breast-health/what-is-breast-cancer-2.
8. Love SM, Gelman RS, Silen W. Sounding board. Fibrocystic "disease" of the breast--a nondisease? New England Journal of Medicine 1982;307(16):1010-4.
9. Poehls UG, Hack CC, Wunderle M, Renner SP, Lux MP, Beckmann MW, et al. Awareness of breast cancer incidence and risk factors among healthy women in Germany: an update after 10 years. Eur. J. Cancer Prev. 2019 Jan 23.
10. Kim DJ, Sun WY, Ryu DH, Park JW, Yun HY, Choi JW, et al. Microglandular adenosis. J Breast Cancer. 2011 Mar; 14(1):72-5.
11. Rosen PP. Microglandular adenosis. A benign lesion simulating invasive mammary carcinoma. Am J Surg Pathol. 1983 Mar; 7(2):137-44.
12. Geyer FC, Kushner YB, Lambros MB, Natrajan R, Mackay A, Tamber N, et al. Histopathology. 2009 Dec; 55(6):732-43.
13. Popper HH, Gallagher JV, Ralph G, Lenard PD, Tavassoli FA. Breast carcinoma arising in microglandular adenosis: a tumor expressing S-100 immunoreactivity. Report of five cases. Breast J. 1996;2:154-9.
14. Pandey PR, Saidou J, Watabe K. Role of myoepithelial cells in breast tumor progression. Front Biosci. 2010 Jan 1;15:226-36.
15. Sharma GN, Dave R, Sanadya J,Sharma P, Sharma KK. Various types and management of breast cancer: An overview. J Adv Pharm Technol Res. 2010 Apr-Jun; 1(2):109-26.
16. Vinay K, Abul KA, Jon CA, Nelson F. Robbins and Cotran Pathologic Basis of Disease. Eight ed. Elsevier; Lyon, France: 2010.
17. Goh CW, Wu J, Ding S, Lin C, Chen X, Huang O, et al. Invasive ductal carcinoma with coexisting ductal carcinoma in situ (IDC/DCIS) versus pure invasive ductal carcinoma (IDC): a comparison of clinicopathological characteristics, molecular subtypes, and clinical outcomes. J Cancer Res Clin Oncol. 2019 Jul;145(7):1877-86.
18. Wallace AS, Xiang D, Hockman L, Arya M, Jeffress J, Wang Z, et al. Synchronous lobular carcinoma in situ and invasive lobular cancer: marker or precursor for invasive lobular carcinoma. Eur J Surg Oncol. 2014 Oct;40(10):1245-9.
19. Lakhani SR, Ellis IO, Schnitt SJ, et al. WHO Classification of tumours of the breast. 4th ed. Lyon, France: IARC Press; 2012. World Health Organization Classification of tumours; vol 4.
20. Li CI, Uribe DJ, Daling JR. Clinical characteristics of different histologic types of breast cancer. Br J Cancer. 2005;93(9):1046-52.
21. Borst MJ, Ingold JA. Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery. 1993;114(4):637-42.
22. Weigelt B, Horlings HM, Kreike B, et al. Refinement of breast cancer classification by molecular characterization of histological special types. J Pathol. 2008;216(2):141-50.
23. Reis-Filho JS, Lakhani SR. Breast cancer special types: why bother? J Pathol. 2008;216(4):394-8.
24. Berg JW, Hutter RV. Breast cancer. Cancer. 1995 Jan 1;75(1 Suppl):257-69.
25. Badowska-Kozakiewicz AM, Patera J, Sobol M, Przybylski J. The role of oestrogen and progesterone receptors in breast cancer – immunohistochemical evaluation of oestrogen and progesterone receptor expression in invasive breast cancer in women. Contemp Oncol (Pozn). 2015; 19(3):220-5.
26. Rosai J. Rosai and Ackerman’s Surgical Pathology. Tenth ed. Elsevier; Lyon, France: 2011. 1694-6.
27. Arpino G, Bardou VJ, Clark GM, Elledge RM. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res. 2004;6(3):149-56.
28. Rakha EA, El-Sayed ME, Powe DG, Green AR, Habashy H, Grainge MJ, et al. Invasive lobular carcinoma of the breast: response to hormonal therapy and outcomes. Eur J Cancer. 2008 Jan;44(1):73-83.
29. May DS,Stroup NE. The incidence of sarcomas of the breast among women in the United States, 1973-1986. Plastic and reconstructive surgery 1991;87,193-4.
30. Olu-Eddo AN, Ugiagbe EE. Benign breast lesions in an African population: A 25-year histopathological review of 1864 cases. Niger Med J. 2011 Oct-Dec;52(4):211-6.
31. Abdallah DM, MF El Deeb N. Comparative immunohistochemical study of P63, SMA, CD10 and Calponin in distinguishing in situ from invasive breast carcinoma. J Mol Biomark Diagn 8: 342.
32. Batistatou A, Stefanou D, Arkoumani E, Agnantis NJ. The usefulness of p63 as a marker of breast myoepithelial cells. In Vivo. 2003 Nov-Dec;17(6):573-6.
33. Sagiroglu J, Tugrul Ozdemir T, Erdogan KO, Ozemir IA, Eren T, Artis T, et al. Benign diseases diseases of the breast: A retrospective study. Conference: SIS 6th Congress of the
Croatian Senologic Society At: Opatija, Croatia. November 2015.
34. Wang Y, Yin Q, Yu Q, Zhang J, Liu Z, Wang S, t al. A retrospective study of breast cancer subtypes: the risk of relapse and the relations with treatments. Breast Cancer Res Treat. 2011 Nov;130(2):489-98.
35. Balekouzou A, Yin P, Pamatika CM, Bishwajit G, Nambei SW, Djeintote M, et al. Epidemiology of breast cancer: retrospective study in the Central African Republic. BMC Public Health. 2016; 16:1230.
36. Mansouri H, Mnango LF, Magorosa EP, Sauli E, Mpolya EA. Ki-67, p53 and BCL-2 expressions and their association with clinical histopathology of breast cancer among women in Tanzania. Sci Rep. 2019 Jul 9;9(1):9918.