Experimental model for the evaluation of metabolic status after gastric bypass in obese rats Experimental rat model in obesity
Main Article Content
Abstract
Objective: Obesity is an exceedingly current pathology with many clinical, molecular, and psychological implications. The number of obese people has doubled in the past ten years, and we can observe an early onset of obesity. Bariatric surgery is an effective treatment for severe obesity and type 2 diabetes mellitus (T2DM); Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are the two most prevalent types of this procedure . Nevertheless, no single mechanism has emerged that thoroughly explains the metabolic benefit and subsequent long-term effects after surgery. Webster's new collegiate dictionary defines the noun model as: 'a descriptive or analogy used to help visualize something that cannot be directly observed.' Sustained by this definition, the animal models in nutritional research are fundamental to improve human conditions. Due to the recent boost in experimental surgery, our aim in this study is to set the main technical characteristics of the gastric bypass operation and specific animal care in the metabolic surgery field we have been undertaking in our center.
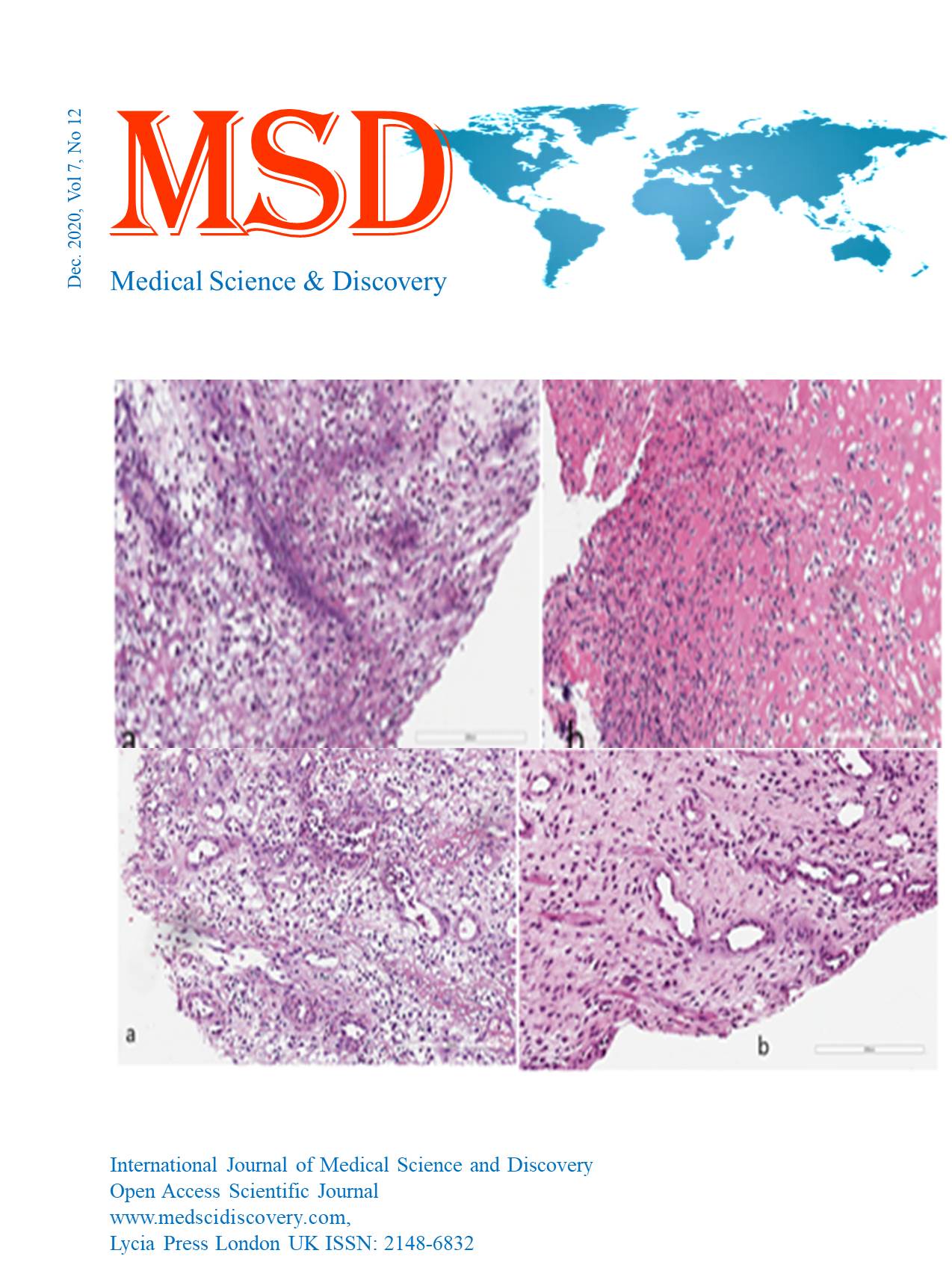
Materials and methods: We chose Wistar rats fed with a high caloric diet (HCD) 82g / 100 g fat, 53/100 g saturated fat, 64/100 g carbohydrates. After 7-15 weeks of this diet, depending on the protocol understudy, a consistent three-fold greater weight gain is achieved than the usual range of the free eating chow. After approximately three months on an HCD, the obese rats manifest biochemical features of the metabolic syndrome.
Results: The weight loss for group B (By-pass) was 125 ± 16.16 g, and for group BS (By-pass + Sulodexid), it was 133.10 ± 14.38 g. Although the weight loss was higher in group BS, it is not statistically significantly higher than in group B (p = 0.345), despite administering a pharmacologically active substance in group BS. Although small (approximately 40-50 g), the difference between the control group and groups B and BS is statistically significant with p = 0.016 and 0.026 and Pearson index of 0.674 and 0.628, respectively. Statistical significance also kept the difference between group C and group S (p = 0.028, Pearson Coefficient = 0.621).
Conclusions: First of all, Metabolic surgery is the most effective weight-loss method and improvement or even remission of some diseases associated with obesity. Like today's high-calorie diet, the diet administered, mostly of adolescents, generates both obesity and its associated diseases: diabetes, hypertriglyceridemia, hypercholesterolism, thus increasing mortality and overall morbidity. Second, metabolic surgery radically improves the parameters targeting obesity (weight,% EBWL) and its associated conditions: diabetes mellitus, hypertriglyceridemia, hypercholesterolemia, strongly associated with decreasing life expectancy of the general population. Parameters targeted by gastric bypass: glycemia, TGL, CHO, hepatic steatosis, testicular atrophy registering significant improvements.
Downloads
Article Details
Accepted 2020-12-16
Published 2020-12-21
References
Boden G, Song W, Pashko L, K. K. (2008) ‘In vivo effects of insulin and free fatty acids on matrix metalloproteinases in rat aorta’, Diabetes, 57(476).
Bouloumié, A. et al. (2001) ‘Adipocyte Produces MMP2 and 9 Involvement in Adipose Differentiation’, Diab, 50(9), pp. 2080–2086.
Booth, H. et al. (2014) ‘Incidence of type 2 diabetes after bariatric surgery: Population-based matched cohort study’, The Lancet Diabetes and Endocrinology. Booth et al. Open Access article distributed under the terms of CC BY, 2(12), pp. 963–968.Broekhuizen, L. N. et al. (2010) ‘Effect of sulodexide on glycocalyx and vascular permeability in patients with type 2 diabetes’, Diabet, 53(12), pp. 2646–2655.
Mirica, R. M. et al. (2017) ‘Quality of Life Assessment After Metabolic Surgery — a Single-Center Experience’. Indian Journal of Surgery.
Mirica, R. M. et al. (no date) ‘The Important Roles of Matrix MMP in the Pathophysiology of Obesity’, pp. 1481–1484.
Mingrone, G. et al. (2015) ‘Metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 Year follow-up of an open-label, single-centre, randomised controlled trial’, The Lancet. Elsevier Ltd, 386(9997), pp. 964–973.
Nickel, F., Schmidt, L., Bruckner, T., Billeter, A. T., et al. (2017) ‘Gastrointestinal Quality of Life Improves Significantly After LSG and RYGB—a Prospective Cross-Sectional Study Within a 2-Year Follow-up’, Obesity Surgery. Obesity Surgery, 27(5), pp. 1292–1297.
Nickel, F., Schmidt, L., Bruckner, T., Büchler, M. W., et al. (2017) ‘Influence of bariatric surgery on qol, body image, and general self-efficacy within 6 and 24 months—a prospective study’, Surgery for Obesity and Related Diseases. Elsevier, 13(2), pp. 313–319.
Nicolae Angelescu, F. P. (2010) Caiet de tehnici chirurgicale.
Noel P, Nedelcu M, Nocca D, Schneck AS, Gugenheim J, Iannelli A, G. M. (2014) ‘Revised sleeve gastrectomy:an option for weight loss failure after LSG’, Surg Endosc, 28(4), pp. 1096–1102.
POPESCU, L.A., VIRGOLICI, B., STEFAN, D.C.A., LIXANDRU, D., TIMNEA, O., VIRGOLICI, H., ORASEANU, D., SINESCU, C., MOHORA, M. (2017) ‘Vascular Reactivity and Proinflammatory Cytokines in the Obese Children’, Rev. Chim.(Bucharest), 68(4), pp. 758–768.
Popov Y, S. D. (2009) ‘Targeting liver fibrosis: strategies for development and validation of antifibrotic therapies’, Hepatology, 50: 1294–3.
Qin DD, Yuan W, Z. W. (2007) ‘Do reproductive hormones explain the association between body mass index and semen quality?’, Asian J Androl, 9, pp. 827–34.
Regan JP, Inabnet WB, Gagner M, P. A. (2003) ‘Early experience with two-stage laparoscopic RYGB as an alternativein the super obese patient.’, Obes Surg., 13(6), pp. 861–864.
Ress, C. et al. (2010a) ‘Influence of significant weight loss on serum MMP-7 levels’, European Cytokine Network, 21(1), pp. 65–70.
Ress, C. et al. (2010b) ‘Influence of significant weight losson serum MMP-7 levels’, European Cytokine Network, 21(1), pp. 65–70.
Reynolds, C. L., Byrne, S. M. and Hamdorf, J. M. (2017) ‘Treatment Success: Investigating Clinically Significant Change in QoL Following Bariatric Surgery’, Obesity Surgery. Obesity Surgery, 27(7), pp. 1842–1848.
Ribaric, G., Buchwald, J. N. and McGlennon, T. W. (2014) ‘Diabetes and weight in comparative studies of bariatric surgery vs conventional therapy:A review and meta-analysis’, Obesity Surgery, 24(3), pp. 437–455.
Sacks, J. et al. (2018) ‘Effect of RYGB on liver mitochondrial dynamics in a rat model of obesity’, Physiological Reports, 6(4), p. e13600.
Salminen, P. et al. (2018) ‘Effect of LSG vs LRYGB on Weight Loss at 5 Years Among Patients With Morbid Obesity’, Jama, 319(3), p. 241.
Santoro, S. et al. (2014) ‘Sleeve gastrectomy with anti-reflux procedures’, Einstein (São Paulo), 12(3), pp. 287–294.
Serra, R. et al. (2014) ‘The effects of sulodexide on both clinical and molecular parameters in patients with mixed arterial and venous ulcers of lower limbs’, pp. 519–527.
Sierżantowicz R1, Lewko J2, Hady HR3, Kirpsza B1, Trochimowicz L3, D. J. (2017) ‘Effect of BMI on quality of life and depression levels after bariatric surgery.’, Adv Clin Exp Med, 26(3), pp. 491–496.