Clinical and histopathological analysis of metastatic brain tumours: A single-centre experience
Main Article Content
Abstract
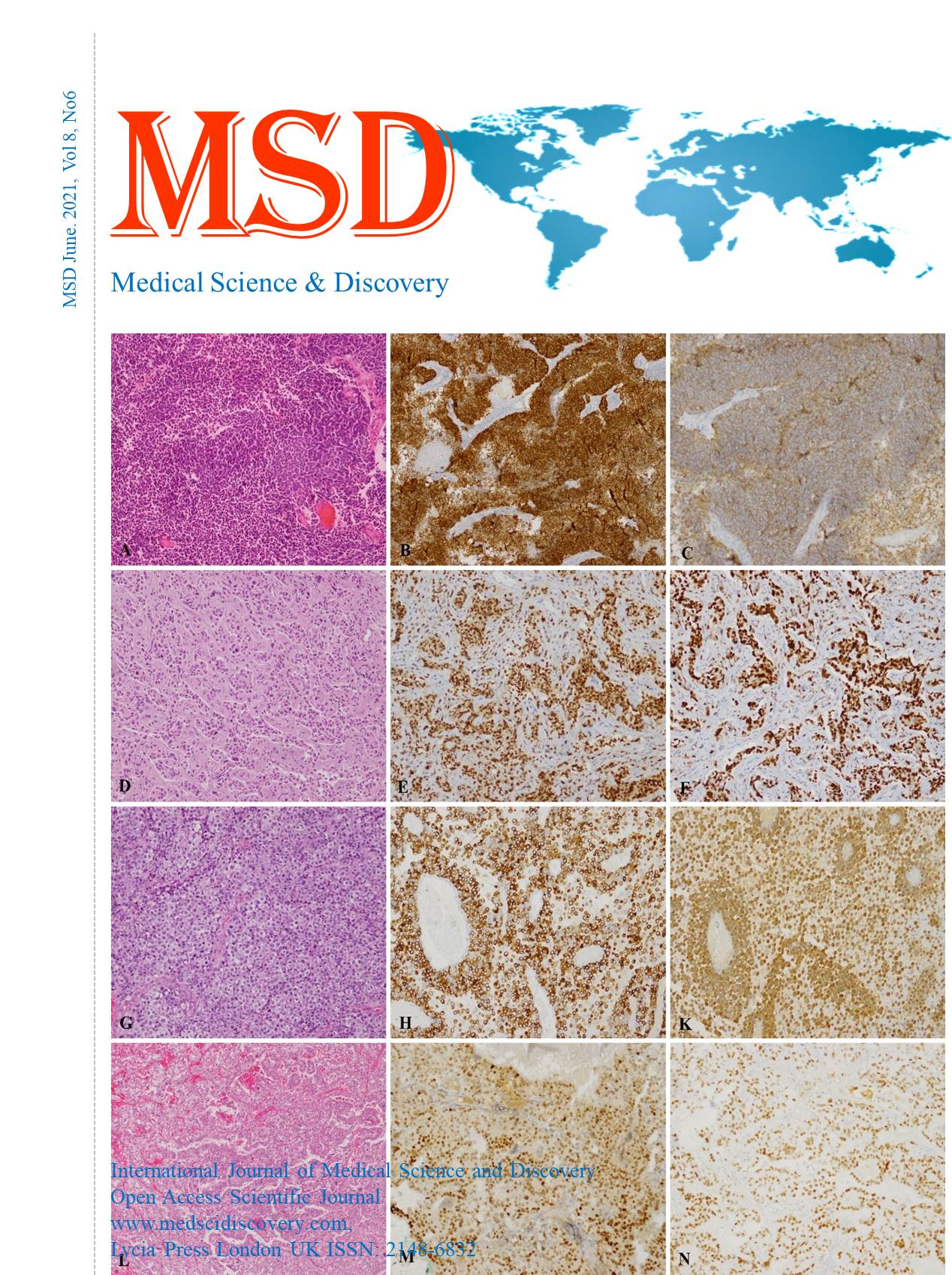
Objective: The aim of this study is to determine the demographic and clinical findings of cases which have been operated for a brain mass and have metastasis, to analyse the histopathological findings, to draw attention to the molecular tests that are effective in the treatment of the primary tumour, and to compare our results with the literature data.
Material and Methods: One hundred seventy cases diagnosed with brain metastasis tumour between January 2012-2021 were analysed retrospectively. The clinical findings and demographic information of the cases were recorded from the hospital information system. The diagnoses of the patients diagnosed with metastasis, the analysis of the cases with or without a primary tumour at the time of diagnosis, and the immunohistochemical staining applied to detect the primary metastasis were recorded.
Results: Sixty-seven of the cases were female, and one hundred three were male. The youngest case was 14, and the oldest case was 90 years old (Mean 55.6 ± 14). While the clinical findings in 35 of the cases were solely headache, 41 patients also had at least one of the symptoms such as dizziness, seizure, weakness, and ataxia in addition to headache. The primary was unknown at the time of diagnosis of brain metastasis in 63 of the cases. There was a single focus in 107 cases, and multiple metastasis focus in 63 patients. Among all cases, lung (84), breast (24) colorectal (15), kidney (9) metastases were the most common. Primary focus could not be detected in 2 of the cases (neuroendocrine carcinoma and adenocarcinoma) despite all imaging techniques as well as immunohistochemical findings.
Conclusion: The possibility of metastasis is also present in cases with a single lesion and whose primary diagnosis is unknown, and histomorphological analysis become inevitable due to the increase in molecular examinations and the development of patient-specific treatment protocols. Besides, it should not be forgotten that the most common tumour-causing brain metastasis -whether or not the primary is known- is the lung. Kidney tumours may also present with metastasis without manifesting themselves.
Downloads
Article Details
Accepted 2021-06-20
Published 2021-06-24
References
Markesbery WR, Brooks WH, Gupta GD, Young AB. Treatment for patients with cerebral metastases. Arch Neurol. 1978; 35(11):754–6.
Lowery FJ, Yu D. Brain Metastasis: Unique Challenges and Open OpportunitiesBiochim Biophys Acta. 2017 January ; 1867(1): 49–57. doi:10.1016/j.bbcan.2016.12.001
Sen M, Demiral AS, Cetingoz R, Alanyali H, Akman F, Senturk D, et al. Prognostic factors in lung cancer with brain metastasis. Radiother Oncol. 1998; 46(1):33–8.
Sperduto PW, Kased N, Roberge D, Chao ST, Shanley R, Luo X, et al. The effect of tumor subtype on the time from primary diagnosis to development of brain metastases and survival in patients with breast cancer. J Neurooncol. 2013; 112(3):467–72.
Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012; 14(1):48–54.
Patchell RA. The management of brain metastases. Cancer Treat Rev. 2003; 29(6):533–40. doi: 10.1016/s0305-7372(03)00105-1.
Ammannagari N, Ahmed S, Patel A, Bravin EN. Radiological response of brain metastases to novel tyrosine kinase inhibitor lapatinib. QJM. 2013;106(9):869–70.
Parker GD, Hamsberger HR. Clinical-radiologic issues in perineural tumor spread of malignant diseases of the extracranial head and neck. Radiogrophics. 1991;11:383-399.
Takei H, Rouah E, Ishida Y. Brain metastasis: clinical characteristics, pathological findings and molecular subtyping for therapepeutic implications. Brain Tumor Pathol. 2016;33:1-12.
Fox BD, Cheung VJ, Patel AJ, Suki D, Rao G. Epidemiology of metastatic brain tumors. Neurosurg Clin N Am. 2011;22(1):1–6. doi: 10.1016/j.nec.2010.08.007.
Chukwueke UN, Brastianos PK. Precision Medical Approaches to the Diagnoses and Management of Brain Metastases Curr. Treat. Options in Oncol. 2019; 20: 49.
Villarreal-Garza C, de la Mata D, Zavala DG, Macedo-Perez EO, Arrieta O. Aggressive treatment of primary tumor in patients with non-small-cell lung cancer and exclusively brain metastases. Clin Lung Cancer. 2013;14:6–13.
Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–46.
Sperduto PW, Chao ST, Sneed PK, Luo X, Suh J, Roberge D, et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multiinstitutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys. 2010;77(3):655–61.
Long GV, Menzies AM, Nagrial AM, Haydu LE, Hamilton AL, Mann GJ, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29(10):1239–46.