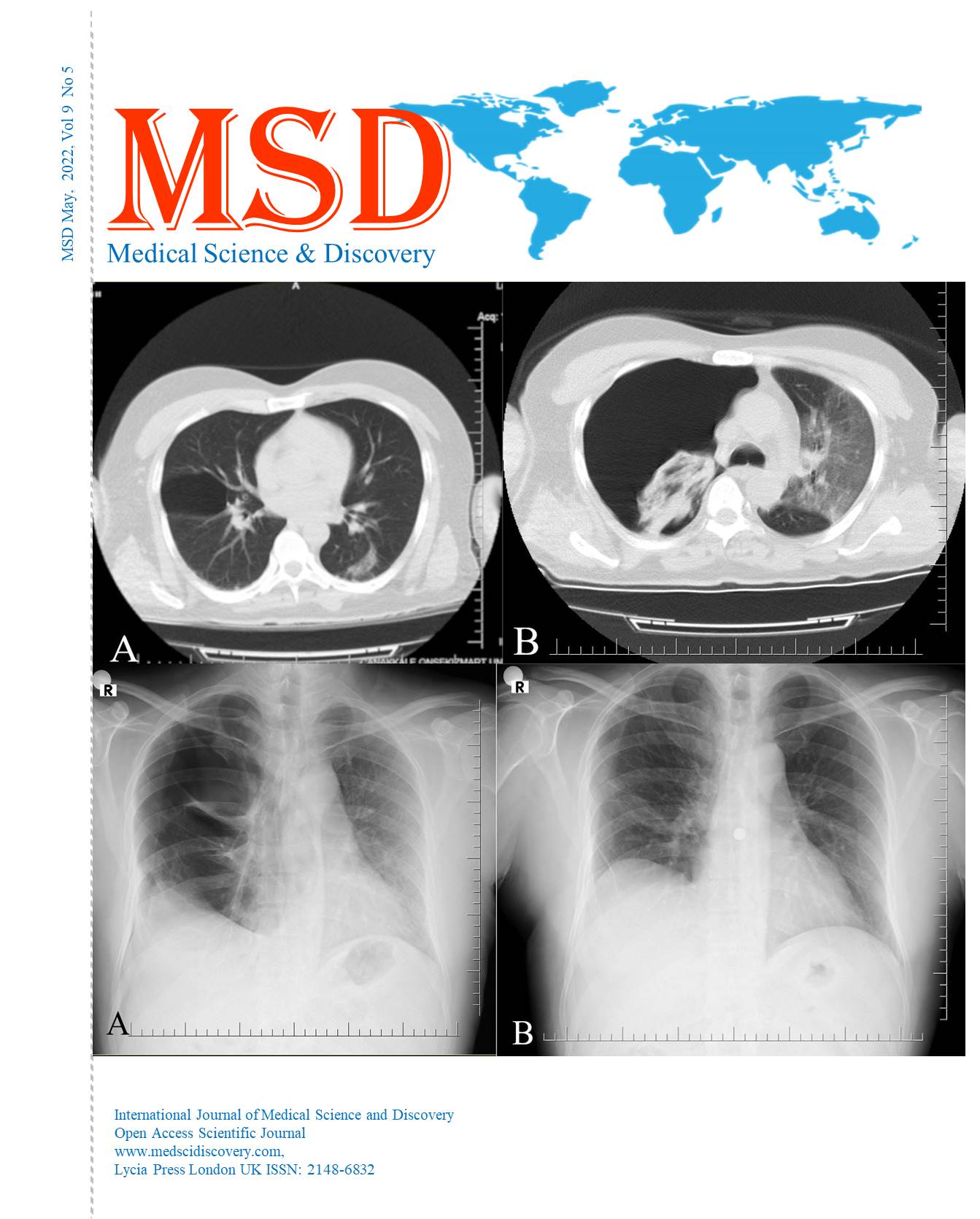
Spontaneous hematomas, the new surgical challenge of COVID patients? Hematomas in COVID patients Hematomas in COVID patients
Main Article Content
Abstract
Objective: There was a critical inconsistency in making therapeutic choices regarding anticoagulation in patients with COVID-19. This study aims to evaluate and determine the causes that led to the formation of hematomas, spontaneous bleeding or what is involved in this hypothesis and the elements related to this aspect.
Patients and methods: The present study is a case series analysis that aims to identify and verify the cause of spontaneous hematomas in COVID positive patients for whom surgery was required. Thus, we analysed patients who presented various spontaneous hematomas during the covid pandemic (March 2020 - May 2021) for which surgery was performed, having as a control group (CG) a homogeneous group in terms of age, covid infection severity, and comorbidities with the study group (SG).
Results: Regarding the preoperative and postoperative days, SG had average values of 4.76±5.36 (Mean±SD) for preoperative days and 9.5±9.327 for postoperative days. Given that one of the most suspected causes of hematomas was considered an anticoagulant overdose, we compared the anticoagulant doses and the type of anticoagulant, so the anticoagulant doses did not show statistically significant differences (0.836±0.294ml in SG versus 0.866±0.343ml in CG with p=0.588). As expected, hemoglobin (Hb) was significantly lower for SG with mean values of 7.266±1.431mg/dl compared to CG that had mean values of 12.9±2.092mg/dl (p=0.001). The correlation between the value of Hb (average value was 12.9 mg/dl, a minimum of 8.7 mg/dl and a maximum of 16.6 mg/dl) and the value of procalcitonin (average value was 0.13, a minimum of 0.02 and a maximum of 0.7) is statistically significant having p=0.012. In SG, hemoglobin can be correlated with ESR (erythrocyte sedimentation rate), p=0.008 and with procalcitonin, p=0.05. Both have a negative correlation explained by a proinflammatory status that can aggravate low hemoglobin levels, but without a direct link to high ESR and procalcitonin values.
Conclusions: The hypothesis of anticoagulant overdose is not supported or verified by the present study, we consider that additional thromboelastography tests are necessary to be able to completely refute it. Mortality did not increase statistically significantly
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Accepted 2022-04-23
Published 2022-05-27
References
Shah A, Donovan K, McHugh A, et al. Thrombotic and haemorrhagic complications in critically ill patients with COVID-19: a multicentre observational study. Crit Care. 2020;24(1):561. Published 2020 Sep18. doi:10.1186/s13054-020-03260-3 DOI: https://doi.org/10.1186/s13054-020-03260-3
Musoke N, Lo KB, Albano J, et al. Anticoagulation and bleeding risk in patients with COVID-19. Thromb Res. 2020;196:227-230. doi:10.1016/j.thromres.2020.08.035 DOI: https://doi.org/10.1016/j.thromres.2020.08.035
Koupenova M, Freedman JE. Platelets and COVID-19: Inflammation, Hyperactivation and Additional Questions. Circ Res. 2020;127(11):1419-1421. doi:10.1161/CIRCRESAHA.120.318218 DOI: https://doi.org/10.1161/CIRCRESAHA.120.318218
Patell R, Chiasakul T, Bauer E, Zwicker JI. Pharmacologic Thromboprophylaxis and Thrombosis in Hospitalized Patients with COVID-19: A Pooled Analysis. Thromb Haemost. 2021;121(1):76-85. doi:10.1055/s-0040-1721664 DOI: https://doi.org/10.1055/s-0040-1721664
Zaidi FZ, Zaidi ARZ, Abdullah SM, Zaidi SZA. COVID-19 and the ABO blood groupconnection. Transfus Apher Sci. 2020;59(5):102838. doi:10.1016/j.transci.2020.102838 DOI: https://doi.org/10.1016/j.transci.2020.102838
Rostami M, Mansouritorghabeh H. D-dimer level in COVID-19 infection: a systematic review. Expert Rev Hematol. 2020;13(11):1265-1275. doi:10.1080/17474086.2020.1831383 DOI: https://doi.org/10.1080/17474086.2020.1831383
Benazzi, D., Antonicelli, V., Presciuttini, B., Foroni, E., Bellini, M., Smurra, A., Lo Bianco, C. and Amato, M., 2021. COVID-19 and hemorrhagic complications: pectoral hematoma - Italian Journal of Emergency Medicine 2021 April;10(1):6-10. DOI: https://doi.org/10.23736/S2532-1285.21.00044-6
Rogani S, Calsolaro V, Franchi R, Calabrese AM, Okoye C, Monzani F. Spontaneous muscle hematoma in older patients with COVID-19: two case reports and literature review. BMC Geriatr. 2020;20(1):539. Published 2020 Dec 22. doi:10.1186/s12877-020-01963-4 DOI: https://doi.org/10.1186/s12877-020-01963-4
Nakamura H, Ouchi G, Miyagi K, et al. Case Report: Iliopsoas Hematoma during the Clinical Course of Severe COVID-19 in Two Male Patients (published online ahead of print, 2021 Jan 13). Am J TropMed Hyg. 2021;104(3):1018-1021. doi:10.4269/ajtmh.20-1507 DOI: https://doi.org/10.4269/ajtmh.20-1507
Bargellini I, Cervelli R, Lunardi A, et al. Spontaneous Bleedings in COVID-19 Patients: An Emerging Complication. Cardiovasc Intervent Radiol. 2020;43(7):1095-1096. doi:10.1007/s00270-020-02507-4 DOI: https://doi.org/10.1007/s00270-020-02507-4
Jahollari A, Cavolli R, Tavlasoglu M, Sallahu F, Muriqi S. Iliopsoas hematoma due to muscular rupture following defibrillation. Ulus Travma Acil Cerrahi Derg. 2013;19(6):564-566. doi:10.5505/tjtes.2013.74152 DOI: https://doi.org/10.5505/tjtes.2013.74152
Ohn MH, Ng JR, Ohn KM, et al Double-edged sword effect of anticoagulant in COVID-19 infection BMJ Case Reports CP2021;14:e241955. DOI: https://doi.org/10.1136/bcr-2021-241955
Sahu KK, Mishra AK, Lal A, George SV, Siddiqui AD. Clinical spectrum, risk factors, management and outcome of patients with retroperitoneal hematoma: a retrospective analysis of 3-year experience (published correction appears in Expert Rev Hematol. 2020 Jun;13(6):i). Expert Rev Hematol. 2020;13(5):545-555. doi:10.1080/17474086.2020.1733963 DOI: https://doi.org/10.1080/17474086.2020.1733963
Charra, Boubaker; Ellouadghiri, Ayman; Kebbou, Touda; Ettouki, Omar; El Benna, Naima; Afif, Moulay Hicham; Gharbi, Mohamed Benghanem. Acute spontaneous hematoma of the corpus callosum in a COVID-19 patient: a case report.Pan Afr Med J ; 38: 263, 2021.
Guo SH, Zhu SM, Yao YX. Giant Retroperitoneal Hematoma During Extracorporeal Membrane Oxygenation in a Patient With Coronavirus Disease-2019 Pneumonia. J Cardiothorac Vasc Anesth. 2020;34(10):2839-2840. doi:10.1053/j.jvca.2020.05.039 DOI: https://doi.org/10.1053/j.jvca.2020.05.039
Charra B, Ellouadghiri A, Kebbou T, et al. Acute spontaneous hematoma of the corpus callosum in a COVID-19 patient: a case report. Pan Afr Med J. 2021;38:263. Published 2021 Mar 15. doi:10.11604/pamj.2021.38.263.28048 DOI: https://doi.org/10.11604/pamj.2021.38.263.28048
González C, Penado S, Llata L, Valero C, Riancho JA. The clinical spectrum of retroperitoneal hematoma in anticoagulated patients. Medicine (Baltimore). 2003;82(4):257-262. doi:10.1097/01.md.0000085059.63483.36 DOI: https://doi.org/10.1097/01.md.0000085059.63483.36
Tabibkhooei, J. Hatam, M. Mokhtari, M. Abolmaali, COVID-19-associated spontaneous subacute subdural haematoma: report of two cases, New Microbes and New Infections, Volume 40, 2021, 100848, ISSN 2052-2975, https://doi.org/10.1016/j.nmni.2021.100848. DOI: https://doi.org/10.1016/j.nmni.2021.100848
Shiraki H, Morishita K, Kishino M, Nakatsutsumi K, Kimura K, Shirai T, Ishizuka M, Miyazaki Y, Aiboshi J, Otomo Y. An Experience of Multiple Hematomas in a Coronavirus Disease-19 Patient Administered with ART-123 and Heparin. Open Access Emerg Med. 2021;13:207-211 https://doi.org/10.2147/OAEM.S302732 DOI: https://doi.org/10.2147/OAEM.S302732
Wool GD, Miller JL. The Impact of COVID-19 Disease on Platelets and Coagulation. Pathobiology. 2021;88(1):15-27. doi:10.1159/000512007 DOI: https://doi.org/10.1159/000512007
Altschul DJ, Unda SR, de La Garza Ramos R, et al. Hemorrhagic presentations of COVID-19: Risk factors for mortality. Clin Neurol Neurosurg. 2020;198:106112. doi:10.1016/j.clineuro.2020.106112 DOI: https://doi.org/10.1016/j.clineuro.2020.106112