The contribution of preoperative MRI evaluation to emergency surgical management of perianal abscesses
Main Article Content
Abstract
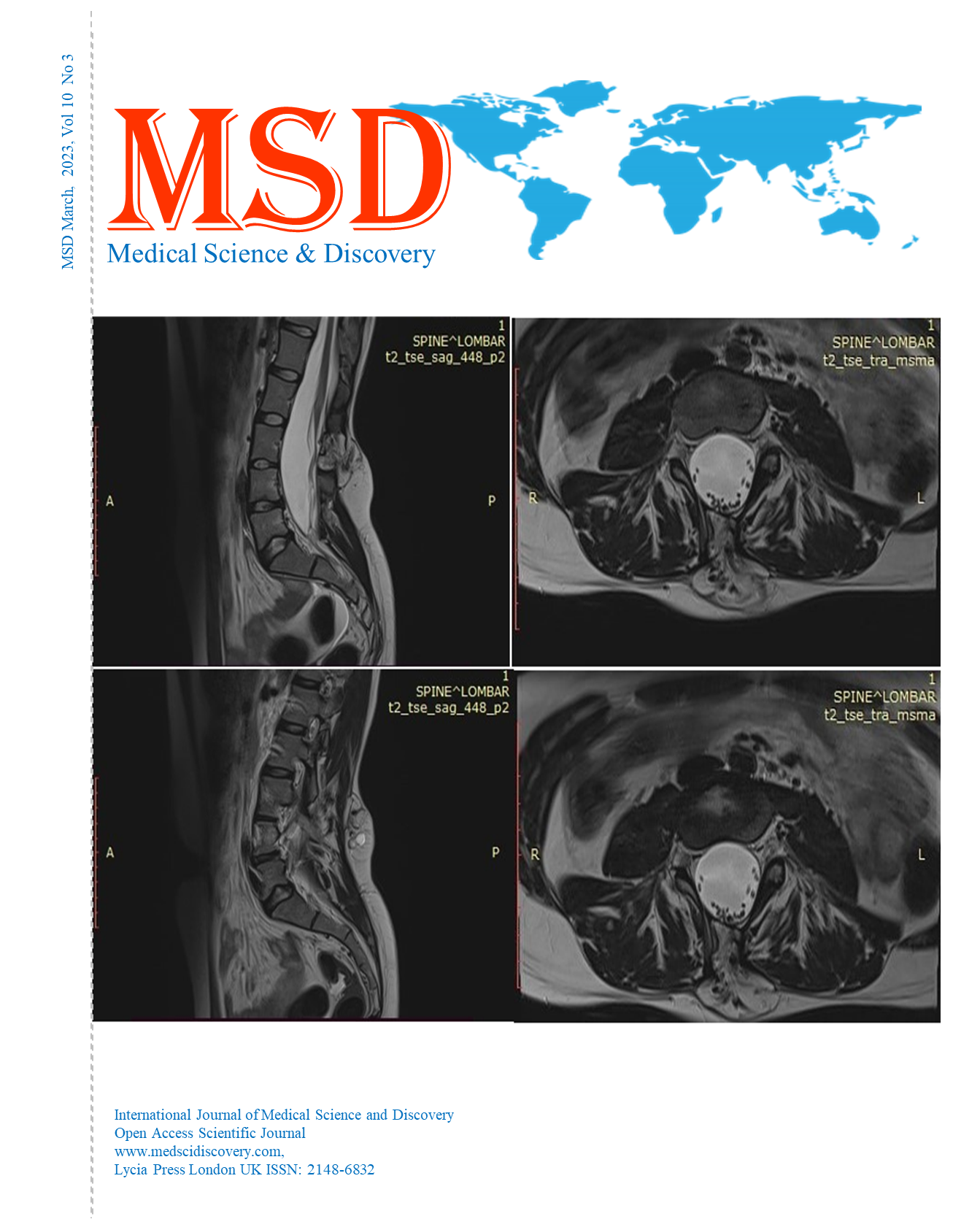
Objective: Perianal abscesses occur as a result of an infection in the anal gland due to the obstruction of the anal gland ducts opening to the anal crypts. Preoperative use of MRI reduces the risk of recurrence, fistula formation, and postoperative fecal incontinence as it allows detailed anatomical imaging. The aim of this study is to investigate the contribution of preoperative MRI to reducing recurrence and surgical complications in patients who underwent emergency surgery for perianal abscess.
Material and Methods: A total of 206 patients with perianal abscess evaluated and not evaluated with MRI between January 2016 and 2021 were included in this retrospective study. The patients had no history of surgery or local drainage applied to the perianal region. In addition to demographic data of patients, postoperative complications, hospitalization duration, recurrence ratio, and MRI findings are evaluated.
Results: In the preoperative period, recurrence was found in 16 (%13.2) of 121 cases evaluated with MRI, while the disease recurred in 24 (%28.2) of 85 cases who were operated without MRI evaluation. The presence of a fistula was significantly higher while the presence of recurrence was significantly lower in the group that underwent MRI in the preoperative period (p=0.033, p=0.012 respectively).
Conclusion: Contrary to popular belief, surgical treatment of abscesses is not that easy due to the high risk of recurrence, the high rate of association with perianal fistula, and the different types and spreads of abscesses. Therefore, preoperative MRI is the most useful diagnostic method for detecting perianal abscesses and additional pathologies.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Accepted 2023-03-14
Published 2023-03-16
References
Abcarian H. Anorectal infection: abscess-fistula. Clin Colon Rectal Surg 2011; 24:14.
Vogel JD, Johnson EK, Morris AM, et al. Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula. Dis Colon Rectum 2016; 59:1117.
Parks AG. Pathogenesis and treatment of fistula-in-ano. BMJ 1961; 1: 463-9.
Zinicola R, Cracco N, Rossi G et al. Acute supralevator abscess: the little we know. Ann R Coll Surg Engl. 2022 Nov;104:645-649. doi: 10.1308/rcsann.2021.0257.
Mercy Jimenez and Nageswara Mandava. Anorectal Fistula. Treasure Island (FL): Stat Pearls (Internet) Last updated: 09.19.2022.
Seow-Choen, Phillips RK. Insights gained from the management of problematical anal fistulae at St. Mark’s Hospital, 1984-88. Br J Surg 1991; 78: 53941.
Panes J, Bouhnik Y, Reinisch W, Stoker J, Taylor SA, Baumgart DC, et al. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis 2013; 7: 556-85.
Steven V. Turner and Jasvinder Singh. Perirectal Abscess. Treasure Island (FL): Stat Pearls (Internet) Last updated: 08.08.2022.
Muller LM, Gorter KJ, Hak E, Goudzwaard WL, Schellevis FG, Hoepelman AI, Rutten GE. Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus. Clin Infect Dis. 2005;41(3):281–288. doi: 10.1086/431587.
Po-Li Wei JJK, Kuo L-J, Lin H-C. Increased risk of diabetes following perianal abscess: a population-based follow-up study. Int J Colorectal Dis (2013) 28. 2012;235-240(28):235–240.
Adamo K, Sandblom G, Brannstrom F, Strigard K. Prevalence and recurrence rate of perianal abscess-a population-based study, Sweden 1997-2009. Int J Color Dis. 2016;31(3):669–673. doi: 10.1007/s00384-015-2500-7.
Cottam DR, Mattar SG, Barinas-Mitchell E, Eid G, Kuller L, Kelley DE, Schauer PR. The chronic inflammatory hypothesis for the morbidity associated with morbid obesity: implications and effects of weight loss. Obes Surg. 2004;14(5):589–600. doi: 10.1381/096089204323093345.
Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC, Payne WG. Obesity and surgical wound healing: a current review. ISRN Obes. 2014;2014:638936–638913. doi: 10.1155/2014/638936.
de Miguel Criado J, del Salto LG, Rivas PF, del Hoyo LF, Velasco LG, de las Vacas MI, et al. MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics 2012; 32: 175-94.
Carvalho LP, Corleta OC, Mallmann ACM, Koshimizu RT, Spolavori A. Neuropatia pudenda: correlação com dados demográficos, índice de gravidade e parâmetros pressóricos em pacientes com incontinência fecal. Arq Gastroenterol 2002;39(3):139-46.
Peña A, Hong AR, Midulla P, Levitt M. Reoperative surgery for anorectal anomalies. Semin Pediatr Surg 2003;12(2):118-23.
Baracho E. Fisioterapia aplicada à obstetrícia, uroginecologia e aspectos de mastologia. 4ª ed. Rio de Janeiro: Guanabara Koogan; 2007.
Sheikh P, Baakza A. Management of Fistula-in-Ano-The Current Evidence. Indian J Surg. 2014;76:482-486.
Halligan S, Stoker J. Imaging of fistula in ano. Radiology 2006; 239: 18-33.
Kuijpers HC, Schulpen T. Fistulography for fistula-in-ano: is it useful? Dis Colon Rectum 1985; 28: 103-4.
Guillaumin E, Jeffrey RB Jr, Shea WJ, Asling CW, Goldberg HI. Perirectal inflammatory disease: CT findings. Radiology 1986; 161: 153-7.
Liang C, Lu Y, Zhao B, Du Y, Wang C, Jiang W. Imaging of anal fistulas: comparison of computed tomographic fistulography and magnetic resonance imaging. Korean J Radiol 2014; 15: 712-23.
Buchanan GN, Halligan S, Bartram CI, Williams AB, Tarroni D, Cohen CR. Clinical examination, endosonography, and MR imaging in preopera-tive assessment of fistula in ano: comparison with outcome-based reference standard. Radiology 2004; 233: 674-81.
Buchanan G, Halligan S, Williams A, Cohen CR, Tarroni D, Phillips RK, et al. Effect of MRI on clinical outcome of recurrent fistula-in-ano. Lancet 2002; 360: 1661-2.
Buchanan GN, Halligan S, Williams AB, Cohen CR, Tarroni D, Phillips RK, et al. Magnetic resonance imaging for primary fistula in ano. Br J Surg 2003; 90: 877-81.
Singh K, Singh N, Thukral C, Singh KP, Bhalla V. Magnetic resonance imaging (MRI) evaluation of perianal fistulae with surgical correlation. J Clin Diagn Res 2014; 8: RC01-4.
Bartram C, Buchanan G. Imaging anal fistula. Radiol Clin North Am 2003; 41: 443-57.