A rare case of high risk multisystem Langerhans Cell Histiocytosis in infant
Main Article Content
Abstract
Objective: Langerhans cell histiocytosis (LCH) stands as the most common histiocytic disorder. It is categorized into single-system single site, single-system multi-site, and multisystem types, with or without involvement of risk organs. Clinical presentation exhibits considerable variability, contingent upon the affected organ systems. Given its rarity, diverse locations, and varying severity, there are currently no established treatment guidelines for LCH.
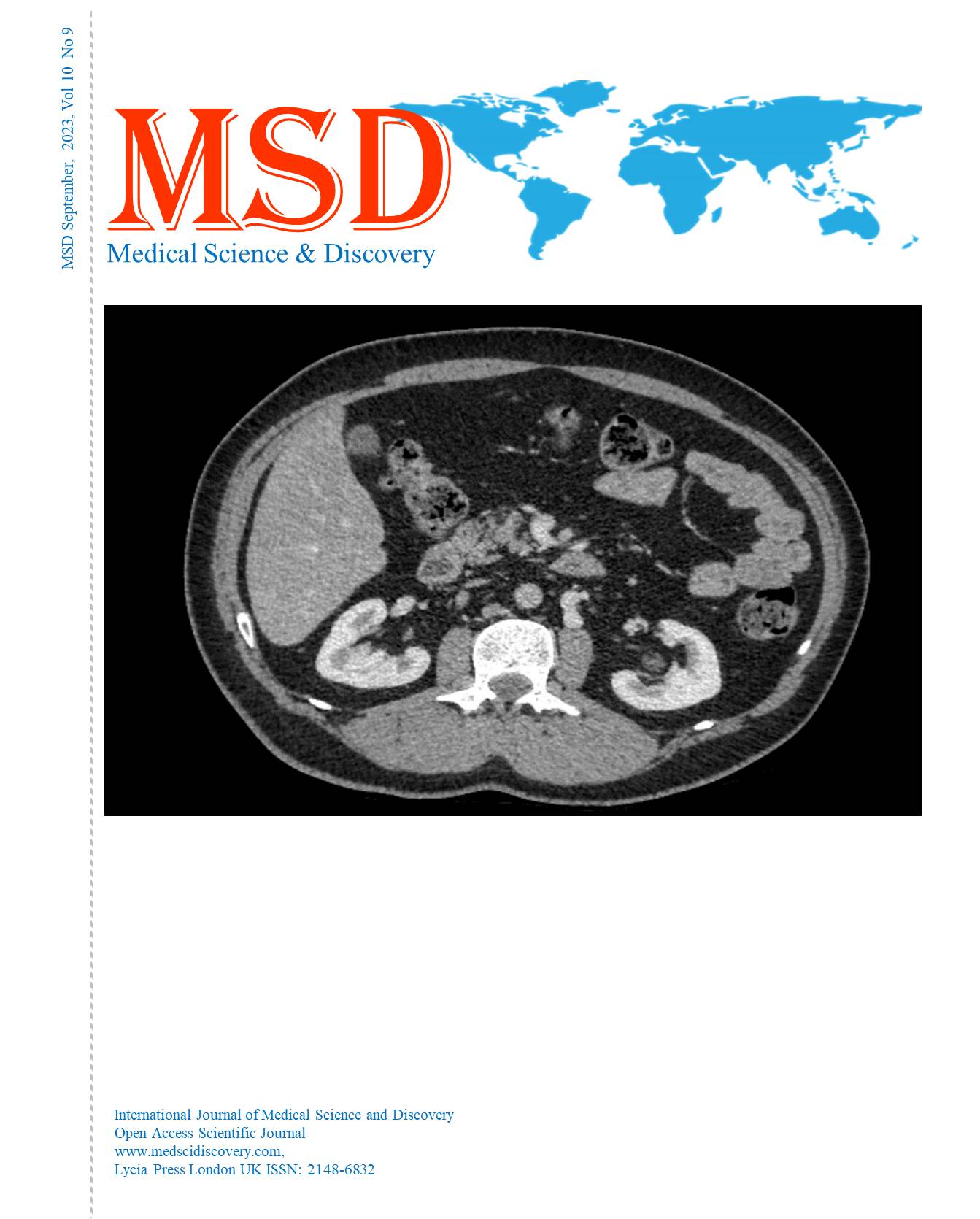
Case Presentation: We documented the case of a 5-month-old male diagnosed with Langerhans cell histiocytosis (LCH), presenting with high-risk multisystem organ involvement and concurrent unifocal bone involvement. Bone marrow aspiration revealed infiltration by multinucleated giant cells within the marrow. Skin biopsy demonstrated Langerhans cell proliferation with epidermotrophism and the characteristic reniform nucleus resembling a coffee bean. The patient was treated following the histiocytosis protocol, which included daily oral prednisone and 6-mercaptopurine, in addition to weekly intravenous vinblastine and methotrexate administered every two weeks. Unfortunately, the patient displayed limited response during the initial phase of treatment and, tragically, passed away during the eighth week of therapy.
Conclusion: Langerhans cell histiocytosis (LCH) is a rare disease characterized by variable disease presentations and is associated with significant morbidity and mortality. Timely recognition of clinical manifestations and risk factors, coupled with appropriate treatment, is crucial to reduce mortality and long-term complications associated with the condition.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Accepted 2023-09-20
Published 2023-09-30
References
Kamal AF, Luthfi AP. Diagnosis and treatment of langerhans cell histiocytosis with bone lesion in pediatric patient: a case report. Ann Med Surg. 2019;45:102-9. DOI: https://doi.org/10.1016/j.amsu.2019.07.030
Lusiana L, Sjakti HA, Rahmayunita G, Jacoeb TN, Krisanti IA. Langerhans cell histiocytosis: diagnosis and management. J Gen Proced Dermatol Venereol Indones. 2019;4(1):17-24. DOI: https://doi.org/10.19100/jdvi.v4i1.161
Rodriguez-Galindo C, Allen CE. Langerhans cell histiocytosis. Blood. 2020;135(16):1319-31. DOI: https://doi.org/10.1182/blood.2019000934
Badalian-Very G, Vergilio JA, Degar BA, MacConaill LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in langerhans cell histiocytosis. Blood. 2010;116(11):1919-23. DOI: https://doi.org/10.1182/blood-2010-04-279083
Haupt R, Minkov M, Astigarraga I, Schäfer E, Nanduri V, Jubran R, et al. Langerhans cell histiocytosis (LCH): guidelines for diagnosis, clinical work-up, and treatment for patients till the age of 18 years. Pediatr Blood Cancer. 2013;60(2):175-84. DOI: https://doi.org/10.1002/pbc.24367
Bohn OL, Teruya-Feldstein J, Sanchez-Sosa S. Skin biopsy diagnosis of langerhans cell neoplasms [Internet]. Skin Biopsy - Diagnosis and Treatment. InTech; 2013 [cited 2023 Apr 13]. Available from: http://doi.org/10.5772/55893 DOI: https://doi.org/10.5772/55893
Gadner H, Minkov M, Grois N, Pötschger U, Thiem E, Arico M, et al. Therapy prolongation improves outcome in multisystem langerhans cell histiocytosis. Blood. 2013;121(25):5006-14. DOI: https://doi.org/10.1182/blood-2012-09-455774
Sedky MS, Hamouda A, Taha H, Zaky I, Hassanain O, El Hemaly A, et al. Outcome of high-risk langerhans cell histiocytosis (LCH) in Egyptian children, does intermediate-dose methotrexate improve the outcome? J Pediatr Hematol Oncol. 2019;41(8):635-43. DOI: https://doi.org/10.1097/MPH.0000000000001314
El Ouali Z, Khoubila N, Cherkaoui S, Rachid M, Lamchahab M, Qachouh M, et al. Langerhans cell histiocytosis in children: a case report and brief review of the literature. PAMJ Clin Med. 2019;1(10). DOI: https://doi.org/10.11604/pamj-cm.2019.1.10.20810
Tuysuz G, Yildiz I, Ozdemir N, Adaletli İ. Kurugoglu S, Apak H, et al. Langerhans cell histiocytosis: single center experience of 25 years. Mediterr J Hematol Infect Dis. 2019;11(1):e2019035. DOI: https://doi.org/10.4084/mjhid.2019.035