Evaluation of Perfusion and Function in Cardiac Radionuclide Imaging in Cases of Heart Failure with Mid-Range Ejection Fraction
Main Article Content
Abstract
Objective: Heart failure with mid-range ejection fraction (HFmrEF) poses a significant clinical challenge due to its diverse etiology and variable prognosis. Patients with HFmrEF exhibit an intermediate level of left ventricular dysfunction, making their management and prognosis less well-defined compared to those with heart failure with reduced ejection fraction (HFrEF) or preserved ejection fraction (HFpEF). Coronary artery disease (CAD) is a common underlying cause of HFmrEF and can further exacerbate myocardial dysfunction under stress conditions. In this study, we aimed to evaluate the change in left ventricular ejection fraction with stress in the presence of coronary artery disease in cases of heart failure with mid-range ejection fraction.
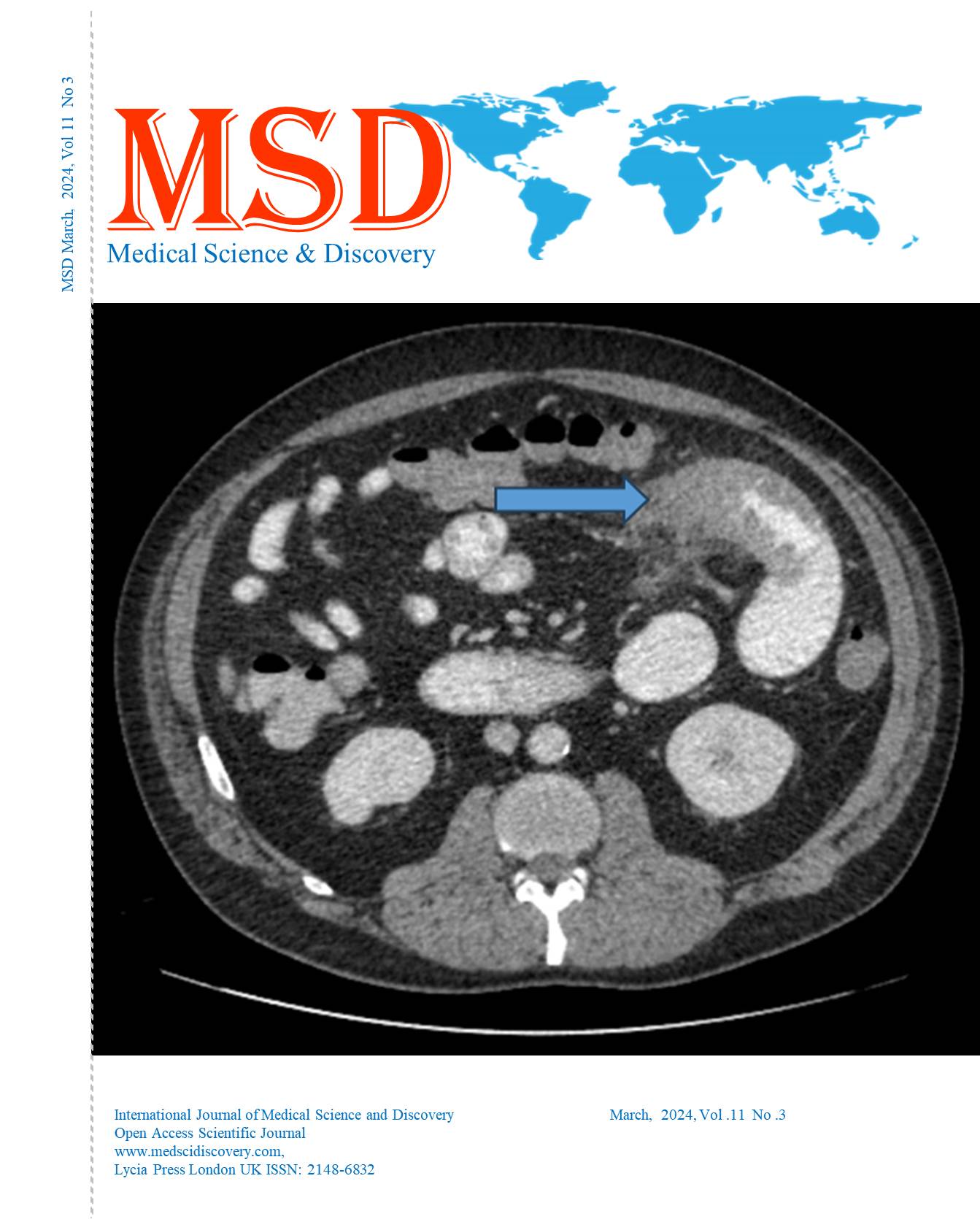
Material and Methods: In this retrospective study, we included 507 patients diagnosed with coronary artery disease and an left ventricular ejection fraction (LVEF) of 41-49% measured by echocardiography. All patients underwent a treadmill exercise test using the Bruce protocol, with progressively increasing speed and incline. Myocardial perfusion was assessed using stress gated myocardial perfusion scintigraphy (MPS), and fixed and reversible defects were identified in cases of coronary artery disease. Cardiac scintigraphic images were acquired from the right anterior oblique to the left posterior oblique. We calculated post-stress LVEF and the percentage decrease in LVEF to evaluate cardiac function.
Results: Resting LVEF was measured as 46 (43-50), while post-stress LVEF was 35 (25-47) in all patients. Myocardial perfusion was evaluated using stress gated MPS in all patients, with 200 (39.5%) patients showing both fixed and reversible perfusion defects. The rate of decrease in LVEF due to stress was significantly higher in patients with reversible perfusion defects (15.90 (6-30.43) vs. 28.26 (24-43.18), p: 0.0005). Post-stress LVEF was lower in patients with reversible perfusion defects (40 (31-47) vs. 33 (25-38), p: 0.0005).
Conclusion: In cases of impaired left ventricular perfusion, quantitative calculations of LVEF may vary, and their reliability may decrease as the ejection fraction decreases under stress conditions. Clinicians should consider this variability in the follow-up of patients with heart failure and mid-range ejection fraction.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Accepted 2024-03-17
Published 2024-03-19
References
Yancy CW, Jessup M, Bozkurt B, et al. ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. American College of Cardiology Foundation. J Am Coll Cardiol. 2013 Oct;62(16):e147-239. Epub 2013 Jun 5.
Kapoor JR, Kapoor R, Ju C, et al. Precipitating Clinical Factors, Heart Failure Characterization, and Outcomes in Patients Hospitalized With Heart Failure With Reduced, Borderline, and Preserved Ejection Fraction. JACC Heart Fail. 2016;4(6):464.
Chioncel O, Lainscak M, Seferovic PM, et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2017;19(12):1574. Epub 2017 Apr 6.
Rickenbacher P, Kaufmann BA, Maeder MT,et al. Heart failure with mid-range ejection fraction: a distinct clinical entity? Insights from the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (TIME-CHF). Eur J Heart Fail. 2017;19(12):1586. Epub 2017 Mar 15.
Koh AS, Tay WT, Teng THK, et al. A comprehensive population-based characterization of heart failure with mid-range ejection fraction. Eur J Heart Fail. 2017;19(12):1624. Epub 2017 Sep 25.
Borlaug BA, Lam CS, Roger VL, et al. Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. J Am Coll Cardiol. 2009 Jul;54(5):410-8.
Schwinger RH, Böhm M, Koch A, et al. The failing human heart is unable to use the Frank-Starling mechanism. Circ Res. 1994;74(5):959.
Komamura K, Shannon RP, Ihara T, et al. Exhaustion of Frank-Starling mechanism in conscious dogs with heart failure. Am J Physiol. 1993;265(4 Pt 2):H1119.
Giannuzzi P, Temporelli PL, Bosimini E, et al. Heterogeneity of left ventricular remodeling after acute myocardial infarction: results of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico-3 Echo Substudy. Am Heart J. 2001;141(1):131.
Rumberger JA, Behrenbeck T, Breen JR,et al. Nonparallel changes in global left ventricular chamber volume and muscle mass during the first year after transmural myocardial infarction in humans. J Am Coll Cardiol. 1993;21(3):673.
Kramer DG, Trikalinos TA, Kent DM,et al. Quantitative evaluation of drug or device effects on ventricular remodeling as predictors of therapeutic effects on mortality in patients with heart failure and reduced ejection fraction: a meta-analytic approach. J Am Coll Cardiol. 2010;56(5):392.
Sabbah HN, Goldstein S. Ventricular remodelling: consequences and therapy. Eur Heart J. 1993;14 Suppl C:24.
Sharov VG, Sabbah HN, Shimoyama H et al. Evidence of cardiocyte apoptosis in myocardium of dogs with chronic heart failure. Am J Pathol. 1996;148(1):141.
Olivetti G, Abbi R, Quaini F, et al. Apoptosis in the failing human heart. N Engl J Med. 1997;336(16):1131.
Weber KT, Pick R, Silver MA,et al. Fibrillar collagen and remodeling of dilated canine left ventricle. Circulation. 1990;82(4):1387.
Sadoshima J, Izumo S . olecular characterization of angiotensin II--induced hypertrophy of cardiac myocytes and hyperplasia of cardiac fibroblasts. Critical role of the AT1 receptor subtype. Circ Res. 1993;73(3):413.
López B, González A, Querejeta R,et al. Alterations in the pattern of collagen deposition may contribute to the deterioration of systolic function in hypertensive patients with heart failure. J Am Coll Cardiol. 2006;48(1):89.
Chancey AL, Brower GL, Peterson JT, et al. Effects of matrix metalloproteinase inhibition on ventricular remodeling due to volume overload. Circulation. 2002;105(16):1983.
Norton GR, Woodiwiss AJ, Gaasch WH,et al. Heart failure in pressure overload hypertrophy. The relative roles of ventricular remodeling and myocardial dysfunction. J Am Coll Cardiol. 2002;39(4):664.
Hayashi M, Tsutamoto T, Wada A, et al. Relationship between transcardiac extraction of aldosterone and left ventricular remodeling in patients with first acute myocardial infarction: extracting aldosterone through the heart promotes ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol. 2001;38(5):1375.
Kelly RA, Smith TW. Cytokines and cardiac contractile function. Circulation. 1997;95(4):778.