KISS1, P53, and PTEN immunoexpressions and prediction of malignancy in endometrial intraepithelial neoplasia lesion within endometrial polyp KISS1, P53 and PTEN in endometrial polyp
Main Article Content
Abstract
Objective: Aim of this study to evaluate the usefulness of phosphase and tensin homologous deleted on chromosome 10 (PTEN), p53, and kisspeptin (KISS1) immunoexpressions in predicting malignancy in endometrial intraepithelial neoplasia within the endometrial polyps.
Material and method: This cross-sectional study was based on chart data from a convenience sample of patients who underwent probe curetage at the Gynecology and Obstetrics Clinic of Başkent University Ankara and Konya Practice and Research Hospitals, Turkey. A total of 169 patients were allocated into 5 groups, comprising the EIN-p group: 62 patients with an endometrial intraepithelial neoplasia lesion within an endometrial polyp, EC group: 17 patients with an endometrial carcinoma, EP-h group: 30 patients with hyperplasia on the background of the polyp but no atypia, EP group: 30 patients with endometrial polyps, and NE group: 30 patients with a normal (proliferative) endometrium. P53, PTEN, and KISS1 expressions between the groups were evaluated.
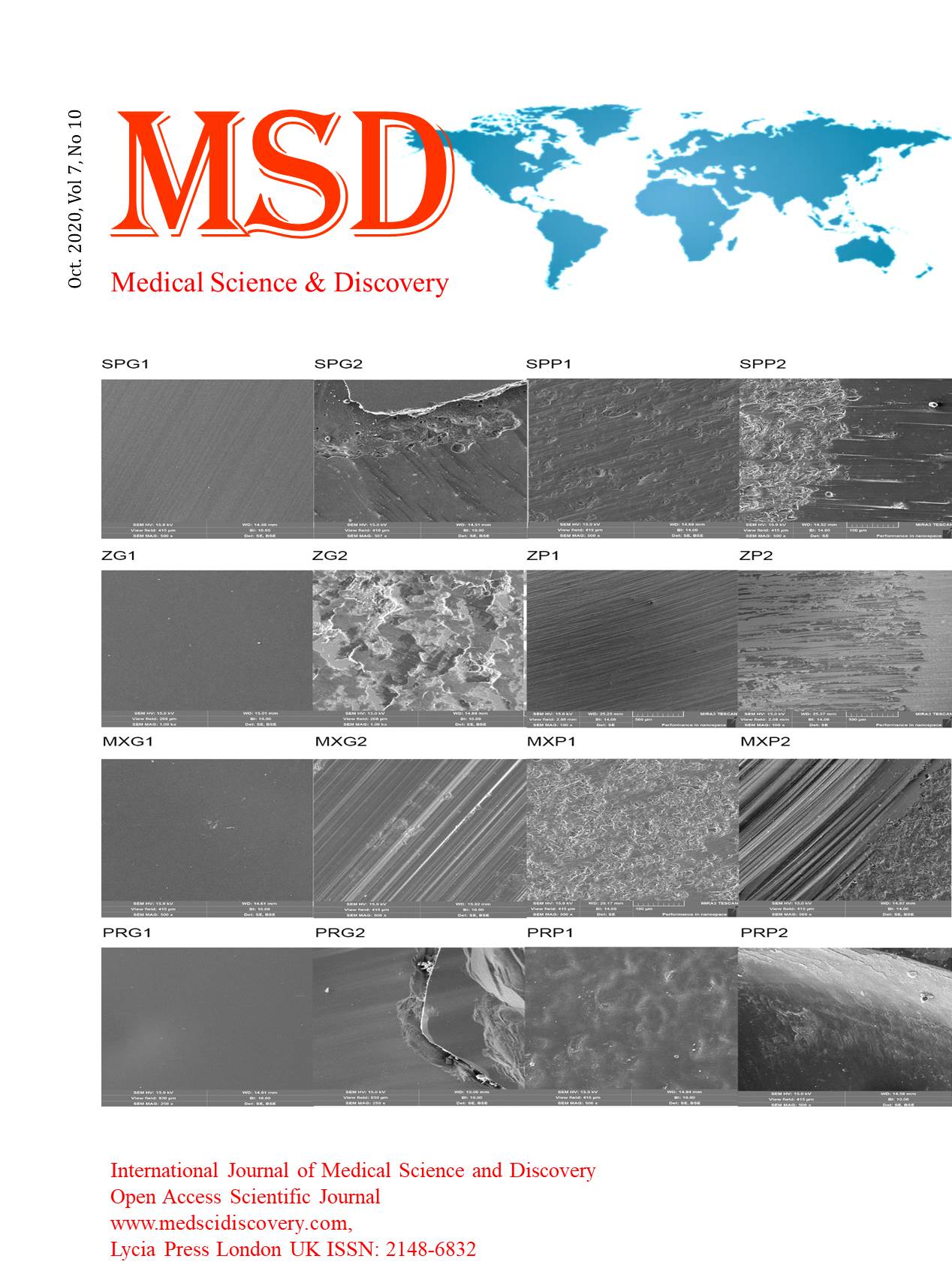
Results: In the EIN-p and EC groups, P53 and KISS1 expressions were moderate or strong. In the NE, EP and EP-h groups, KISS1 was weakly stained and P53 expression was negative. The number of patients with strong p53 and KISS1 expressions in the EC group was higher and this difference was statistically significant (P < 0.001). With PTEN immunostaining, the EC and EIN-P groups were weakly stained, whereas the NE, EP, and EP-h groups had moderate or strong staining. Strong staining rates were higher in patients in the NE and EP groups than in the EP-h group (P < 0.001).
Conclusion: In addition to the literature about P53 and PTEN, according to the data obtained herein, it was speculated that KISS1 may play an important role in the malignant transformation of endometrial polyps and it might be used as a predicting marker in this patient group.
Downloads
Article Details
Accepted 2020-10-06
Published 2020-10-15
References
Savelli L, De Iaco P, Santini D, et al. Histopathologic features and risk factors for benignity, hyperplasia, and cancer in endometrial polyps. Am J Obstet Gynecol. 2003;188(4):927-31.
Lieng M, Istre O, Sandvik L, Qvigstad E. Prevalence, 1-year regression rate, and clinical significance of asymptomatic endometrial polyps: cross-sectional study. J Minim Invasive Gynecol. 2009;16(4):465-71.
Litta P, Di Giuseppe J, Moriconi L, et al. Predictors of malignancy in endometrial polyps: a multi-institutional cohort study. Eur. J. Gynaecol. Oncol. 2014; 35: 382.
Kurman RJ, Carcanglu ML, Herrington CS, et al. WHO Classification of Tumours of Female Reproductive Organs. Lyon, France: IARC Press; 2014. World Health Organization Classification of Tumours; vol 6.
Hayes MP, Ellenson LH. Molecular alterations in uterine serous carcinoma. Gynecol Oncol. 2010;116(2):286–289
Hayes MP, Wang H, Espinal-Witter R, et al. PIK3CA and PTEN mutations in uterine endometrioid carcinoma and complex atypical hyperplasia. Clin Cancer Res. 2006;12(20, pt 1):5932–5935.12–14
Abrao F, Modotti WP, Spadoto-Dias D, et al. Concomitant p53 and PTEN immunoexpression to predict the risk of malignancy in endometrial polyps. Medicine (Baltimore). 2018;97(38):e12304.
Shor S, Pansky M, Maymon R, et al. Prediction of Premalignant and Malignant Endometrial Polyps by Clinical and Hysteroscopic Features. J Minim Invasive Gynecol. 2019;26(7):1311-5.
Athanassiadou P, Athanassiades P, Grapsa D, et al. The prognostic value of PTEN, p53, and beta-catenin in endometrial carcinoma: a prospective immunocytochemical study. Int J Gynecol Cancer. 2007;17(3):697-704.
Appel ML, Edelweiss MI, Fleck J, et al. P53 and BCL-2 as prognostic markers in endometrial carcinoma. Pathol Oncol Res. 2008;14(1):23-30.
Gil A, Rodriguez-Escudero I, Stumpf M, et al. A functional dissection of PTEN N-terminus: implications in PTEN subcellular targeting and tumor suppressor activity. PLoS One. 2015;10(4):e0119287.
Jiang T, Zhang SL, Lin B, et al. [Expression and clinical significance of KISS-1 and GPR54 mRNA in endometrial carcinoma]. Zhonghua Zhong Liu Za Zhi. 2005;27(4):229-31.
Schmidt E, Haase M, Ziegler E, et al. Kisspeptin-10 inhibits stromal-derived factor 1-induced invasion of human endometrial cancer cells. Int J Gynecol Cancer. 2014;24(2):210-7.
Guzman S, Brackstone M, Radovick S, et al. KISS1/KISS1R in Cancer: Friend or Foe? Front Endocrinol (Lausanne). 2018;9:437.
Garg K, Broaddus RR, Soslow RA, et al. Pathologic scoring of PTEN immunohistochemistry in endometrial carcinoma is highly reproducible. Int J Gynecol Pathol. 2012;31(1):48-56.
Li L, Tian J, Zhou L, et al. Role of kisspeptin/GPR54 in the first trimester trophoblast of women with a history of recurrent spontaneous abortion. Int J Clin Exp Pathol. 2017;10(8):8161-73.
Colombo N, Creutzberg C, Amant F, et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, Treatment and Follow-up. Int J Gynecol Cancer. 2016;26(1):2-30.
Yang HP, Meeker A, Guido R, et al. PTEN expression in benign human endometrial tissue and cancer in relation to endometrial cancer risk factors. Cancer Causes Control. 2015;26(12):1729-36.
Adomaitiene L, Nadisauskiene R, Nickkho-Amiry M, et al. Tumor Suppression in Asymptomatic Postmenopausal Endometrial Polyps. Anticancer Res. 2020;40(2):789-94.
Garg K, Leitao MM Jr, Wynveen CA, et al. p53 overexpression in morphologically ambiguous endometrial carcinomas correlates with adverse clinical outcomes. Mod Pathol. 2010;23(1):80–92.
Hayes MP, Wang H, Espinal-Witter R, et al. PIK3CA and PTEN mutations in uterine endometrioid carcinoma and complex atypical hyperplasia. Clin Cancer Res. 2006;12(20, pt 1):5932–5935.12–14
Maia Jr H, Maltez A, Athayde C, et al. P53 expression in spontaneous and estradiol induced hyperplasia during menopause. Maturitas 2003;44:175– 180.
Quddus MR, Sung CJ, Zheng W, et al. P53 immunoreactivity in endometrial metaplasia with dysfunctional uterine bleeding.Histopathology 1999;35:44– 49.
Ryan KM, Phillips AC, Vousden KH. Regulation and function of the p53 tumor suppressor protein. Curr Opin Cell Biol 2001;13: 332– 337.
Jiang Z, Xu W, Dan G, et al. P53 and murine double mimute 2 (MDM2) expression changes and significance in different types of endometrial lesions. Medical science monitor: international medical journal of experimental and clinical research. 2016; 22: 4786.
Okugawa Y, Inoue Y, Tanaka K, et al. Loss of the metastasis suppressor gene KiSS1 is associated with lymph node metastasis and poor prognosis in human colorectal cancer. Oncol Rep. 2013;30(3):1449-54.
Cao F, Chen L, Liu M, et al. Expression of preoperative KISS1 gene in tumor tissue with epithelial ovarian cancer and its prognostic value. Medicine (Baltimore). 2016;95(46):e5296.